Solving Anna Karenina’s COVID-19 Puzzle Part 3 :The Wisdom of Bodhisattva
To cover all the earth with sheets of leather—
Where could such amounts of skin be found?
But with the leather soles of just my shoes
It is as though I cover all the earth! . . .
SHANTIDEVA (685-763)
Bodhicaryavatara: The Way of the Bodhisattva
A long time ago, there lived a king who loved his land and his people very much. His favorite thing to do was to wander all over his kingdom, meeting his subjects and finding out what they needed. It made him happy to help. His only problem was that his blistered feet would ache and bleed from walking everywhere barefoot. It was painful.
One day on the road the kind king met a little girl. The girl asked the king how he was feeling, and the king replied, “Oh, I am very happy. All day long I wander my kingdom granting my subjects’ wishes. The only problem is my feet really hurt! What to do?” The king thought for a moment. Then his eyes lit up and he continued, “I hereby decree that the land shall be covered with leather so my feet will be protected.”
Can you imagine that? So much work, and no flowers would be able to grow! Luckily, the little girl was very wise and kind. She made the king a pair of slippers so he could cover his feet instead. From that day on, he was able to help everyone without hurting his feet.1
What Does This Have to do with COVID-19?
If we look across the World most nations have adopted the strategy of a “General lock-down” to manage the COVID crisis. Essentially putting a stop to almost all human activity – with rather drastic impact on the economic wellbeing of people, specially the small businesses and low income class who have neither the savings to survive nor the real estate to “social distance” themselves. They, in many cases, ended up both poor and infected.
Have we missed the opportunity for sensible segmentation? Or as in the tale of the barefoot King from Shantideva have we tried to cover the earth with leather instead of just making shoes for those who need them most?
We all know by now that COVID-19 is out there and is potentially going to be with us for a long time. It’s also clear that the magnitude of the task in testing all citizens or vaccinating them is extremely daunting and not a practical solution.
In my view the way forward is to focus on that where we are most vulnerable and where can have an impact yet releasing human energy towards repairing the economy as quickly as we can.
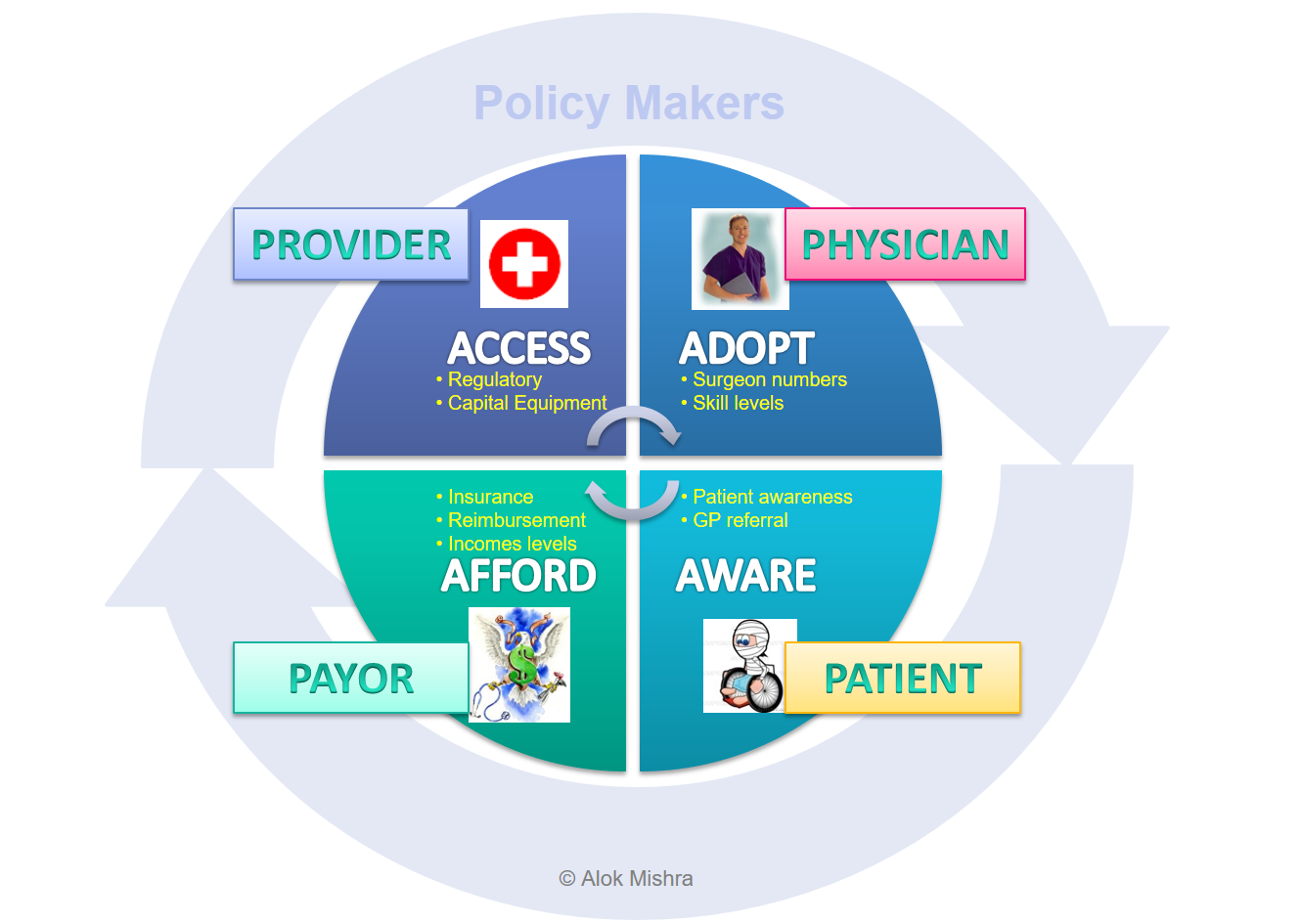
The COVID 19 crisis is not a medical problem any longer. It’s a delicate balance between health and economics and needs each of the 5 stakeholders to understand and play their role in a coordinated way to bring the economy back to health before it goes into shock! It can’t be left to Government alone!
So What Do We Do Now?
Step 1 : Segregate the vulnerable from the robust :
As a first step we need to rethink the lock down and quarantine strategy and segment and segregate people into three groups:
Group 1 Patients with COVID-19
Action : Hospitalise
Group 2 : Vulnerable People (Above 65, obese, heart conditions, diabetes etc)
Action : Quarantine/Lock down and look after using group 3 with hospital like infection control protocols in place. Prioritise them for vaccination as soon as we have a viable product.
Group 3 : Healthy/Asymptomatic
Action : Allow them to go back to work but manage rigorously their interface with group 2. This may help build herd immunity and we could potentially utilise their services to take care of Group 1 & 2 and relieve the burden of Healthcare Practitioners.
Step 2 : Setup multi-stakeholder team with constant communication and transparent access to metrics
Provider
Constantly monitor infrastructure/supplies vs hospital/ICU occupancyRaise alarm bells to Policymaker if saturation is near
Physician
Redirect Healthcare workers to caring for sick patientsEnable GPs to test/prescribe quarantine measures to PatientsInvolve community ( People) in creating capacity for quarantine of vulnerable people
People/Patient
Shift responsibility back to People with demographics/health-profile based guidelinesInvolve People (Community) in creating quarantine capacity away from hospitals and vulnerable population
Policymaker
Constantly monitor infrastructure/supplies vs hospital/ICU occupancy and tighten/open up based on capacity to care Fund care regardless of economic status to avoid re-infection ( Payer)
Payer
Ensure cost of testing, vaccination & care is born by the State ( Policymaker) to avoid affordability-based infections/deaths

Step 3 : Setup metrics for tracking demand vs supply at various capacity bottlenecks : Infrastructure, Supplies, Doctors, Nurses, Finances
The key metrics to be tracked are:
Hospitalization Capacity (H) : Number of additional patients I can take everyday given my resources : Beds, Ventilators, Doctors, Nurses, Money (see discussion on 4A’s)
Patient Flow (P) : Number of sick patients coming in for hospitalisation every day
The moment P starts getting within 80% of H there is a need to set up emergency talks to increase capacity and/or impose stricter lock downs..
In summary recognizing that we still don’t have a vaccine or an effective treatment and the fact that a large proportion of people are immune or have few symptoms a logical solution would be to segregate and protect the vulnerable while allowing the rest of the economy to go back to normal. We will still need to practice hygiene, safe distancing etc but in a practical and not a paranoid way. And mostly when dealing with the vulnerable segment.
We need to wear shoes. Not to cover the earth with leather!
© Alok Mishra, May 21, 2020, All Rights Reserved